Alyssa Clark, Agustina Leiva, Sheilla Muligande, Obafemi Osunmakinde, Allison Rozak▫ Western Reserve Academy, Hudson OH
Reviewed on 6 May 2023; Accepted on 13 July 2023; Published on 16 October 2023
With help from the 2023 BioTreks Production Team.
Every year, an estimated 7 to 12 million people are affected by burn wounds and require medical treatment. Although specialists treat burn patients with widely used bandages and dressings, most patients do not receive adequate treatment. Collagen is a structural protein connecting various human tissues and helps restore the skin’s structure following trauma. A study found that the collagen levels in tilapia fish skin produce a more effective method than traditional bandage treatments. However, collagen levels vary from fish to fish, leading to inconsistent responses to patient treatment. Tilapia also contains several species of opportunistic pathogens that may cause infections. Pseudomonas fluorescens naturally produces a mupirocin antibiotic, which attacks Staphylococcus aureus, a bacterium that commonly causes infections in burn wounds. In this study, we aimed to transform the Scl2 gene, which produces human-like bacterial collagen in Streptococcus pyogenes, into P. fluorescens using a plasmid with demonstrated transformation efficiency and protein production. After the successful transformation, P. fluorescens was synthesized with mupirocin and collagen. We cultured P. fluorescens in a chemostat chamber, which was then harvested and continuously produced collagen and mupirocin. Based on their molecular size, these byproducts went through crossflow filtration to remove collagen and mupirocin. The Bradford assay method was used to measure the collagen concentration in our solution, and the microbiological assay method was used to measure mupirocin concentration. We will create a bandage for burn wounds using this isolated solution. The bandage will help regenerate the skin while minimizing the risk of infection.
Keywords: Collagen, burn wounds, skin treatment, topical treatment, cruelty-free medicine
Authors are listed in alphabetical order. Beth Pethel from Western Reserve Academy, Hudson OH mentored the group. Please direct all correspondence to pethelb@wra.net.
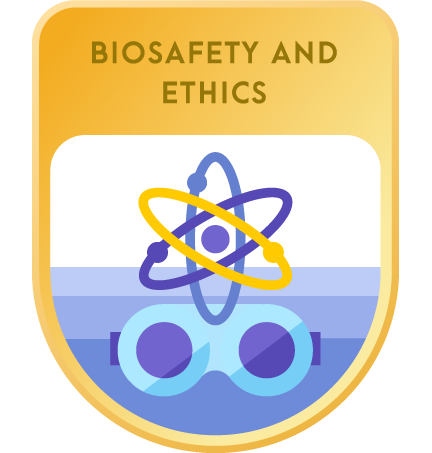
Nearly 33,000 people sustain burn wounds that require medical assistance daily (Stewart, 2022). Burn wounds are injuries to the skin or other organic tissues occurring from heat, radiation, electrical currents, or chemical contact (World Health Organisation, 2018). Based on severity of the burn, there are three degrees of burn wounds: first, second, and third (Figure 1).
| Figure 1. A graphic representation of the various degrees of burns and how they affect the different layers of skin. |
There are three degrees of burn wounds including first, second, and third degrees (Figure 1). First-degree burns are typically superficial and only affect the first layer of skin, the epidermis. This type of burn does not usually require medical assistance. Symptoms often include pain, redness, and swelling. Second-degree burns cause damage to the middle layer of the skin, the dermis, which is a thick underlayer below the epidermis (UC San Diego Health, n.d.). These burns cause swelling, splotchy skin, and painful blisters. With these burns, an individual would need immediate medical attention (Mayo Clinic, 2022). Third-degree burns, the highest severity of burns, extend to the innermost fat layer called the hypodermis, which lies above the muscle and bone (Stanford Medicine, n.d.).
Burn wounds are typically treated with wound dressings, topical and water-based treatments, and skin grafting to reduce damage to the wound area during dressing changes (Mayo Clinic, 2022). Initial water-based treatments involve running cool water on the wound within the first three hours of getting the burn. Topical treatments include antimicrobial ointments, such as silver sulfadiazine, which contains activated silver, an antimicrobial agent (Mayo Clinic, 2022). Skin grafting, a transplant procedure that replaces burned skin with healthy skin, is often required to treat second and third-degree burns (University of Utah Health, n.d.).
The skin used for grafting can be taken from other body parts of the patient, a donor, or even another species (Conde, 2019). In extreme cases, tangential excision surgical methods are required, which remove burned tissue until a layer of viable tissue is encountered. This method prevents the accumulation of bacteria in dead skin and helps new skin to regenerate faster (Phelan & Bernal, 2022). For severe third-degree burns, medical treatments such as ultrasound mist therapy (i.e., low-energy and intense ultrasounds) are delivered through a saline mist that penetrates deep into the wound to kill bacteria (Attinger, 2013). Intravenous (IV) fluids – which help maintain capillary blood flow in the burned tissue – are also used during the healing process (Gauglitz & Williams, 2022).
Regardless of treatment, burn wounds carry a significant risk of excessive blood loss, shock, and deadly infections (Lacey, 2022). To avoid infection, doctors recommend pre-treatment with tetanus shots and antibiotics, which could be applied directly to the skin and taken orally or intravenously (Wiktor & Richards, 2021). With the various methods of healing burn wounds, this study centers on collagen, a critical component for burn wound healing that stimulates new tissue growth (Mazzei, n.d).
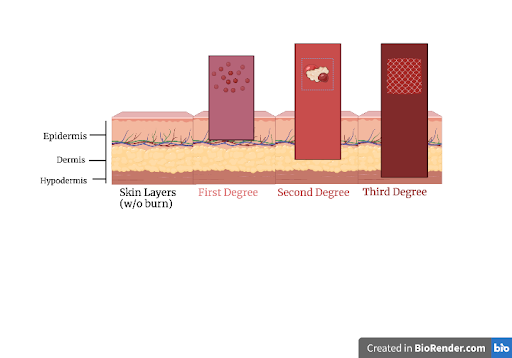
Collagen is a protein that provides structural support for connective tissue, skin, bone, cartilage, and tendons (McIntosh, 2023). It is a critical component of the extracellular matrix (ECM), a network of proteins, RNA, and polysaccharides that help cells attach to and communicate with nearby cells, thereby contributing to cell growth and movement (Figure 2) (Extracellular Matrix, n.d.). There are many different types of collagen that are found in the skin, cartilage, muscles, and cornea among other regions of the body. Type I collagen, the most abundant in the human body, can be turned into collagen-based nanofibers. This makes type I collagen a beneficial solution because of its unique ability to promote cellular proliferation, adhesion, and non-toxicity (Kubala, 2022). When applied to organs and tissue, the type I collagen molecules arrange into long, thin fibrils that form stable interactions, otherwise known as cross-links, in the spaces between cells (Figure 3). The cross-links make strong type I collagen fibers and strengthen skin and muscle tissue (Henriksen & Karsdal, 2016). The bacterial collagen gene, Scl2, contains similar properties as type 1 collagen, including regenerative properties for skin (Collagen, 2022).
| Figure 2: The role of collagen in the extracellular matrix (ECM). |
In 2018, doctors and researchers in Brazil investigated the potential use of tilapia fish skin to heal burn wounds more efficiently than previous methods due to their abundance of Type I collagen. The fish skin helps return the body to its normal state using anti-infective, anti-inflammatory, antifibrotic, and analgesic properties (Fleck & Simman, 2011; Whitaker & Garcia, 2017). Doctors apply the fish skin directly to the burn wound during the treatment. Although the tilapia fish skin treatment costs significantly less than a traditional cream treatment, each tilapia fish varies in the amount of Type I collagen it carries (Lima-Junior et al., 2021) (Deane et al., 2020). Previous research has demonstrated that levels of collagen in tilapia fish skin ranges from as low as 30% to above 40% (Song et al., 2019). Therefore, some patients receive less collagen treatment and have a less efficient healing process than those receiving higher collagen levels (Deane et al., 2020).
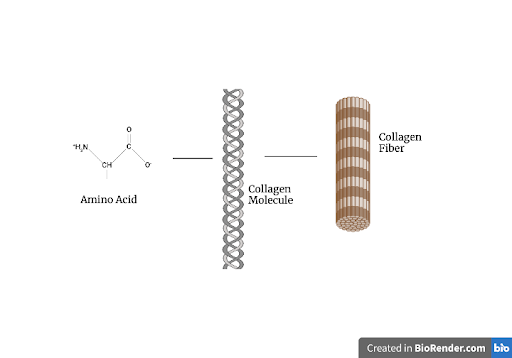
| Figure 3. The structure of collagen including Amino acids (left) that form a triple helix structure that binds to form a collagen fiber. |
Additionally, the fish skin carries opportunistic pathogens such as Aeromonas hydrophila and Streptococcus iniae, which can result in deadly skin infections (Seafish, n.d.). The skin undergoes several sterilization processes and microbiological tests that still have not been proven to be fully effective, all before the skin is ready for any medical processes (Lima-Junior et al., 2019). Furthermore, the availability of antibacterial fish skin grafts only meets 1% of the demand in Brazil (Sussman, 2017). The excessive use of tilapia skin is unsustainable and difficult to mass-produce, as a single fish can only cover thirty-three square centimeters of a burn (Florida Fish and Wildlife Conservation Commission, n.d.). On average, Brazilian physicians used three tilapia fish for a single burn wound, meaning that a third-degree burn wound requires three tilapia fish to cover the area of the wound (Lima-Junior et al., 2019). As the field of medicine strays from the over usage of animals in medical therapies, tilapia fish is a step back from the ethical treatment of burn wounds. Tilapia fish cannot be relocated to new bodies of water as a result of their invasive nature, so the growth in demand for tilapia fish skin cannot be internationally fulfilled (Florida Springs Institute, n.d.).
This project aimed to innovate the treatment of second and third-degree burn wounds by creating a low-cost, cruelty-free solution. Streptococcus pyogenes, a species of gram-positive bacteria, utilizes the Scl2 gene responsible for making collagen that aids the bacterium’s infectivity in its host (Fischetti, 2019). This gene is very similar to human-type I collagen because of its triple-helical structure that maintains stability in human body temperatures, which makes it viable for human wound treatment (Xu et al., 2002).
P. fluorescens, a bacterium that naturally produces mupirocin, will also mass-produce collagen. Mupirocin is one of the most effective antibiotics in terminating S. aureus, a chief causative agent of infections in burn wounds. We will insert the Scl2 gene into P. fluorescens using the pSW002-PpsbA_mTurquoise2 plasmid (Figure 4) because prior experiments have had effective transformations for protein purification in this specific bacterium.
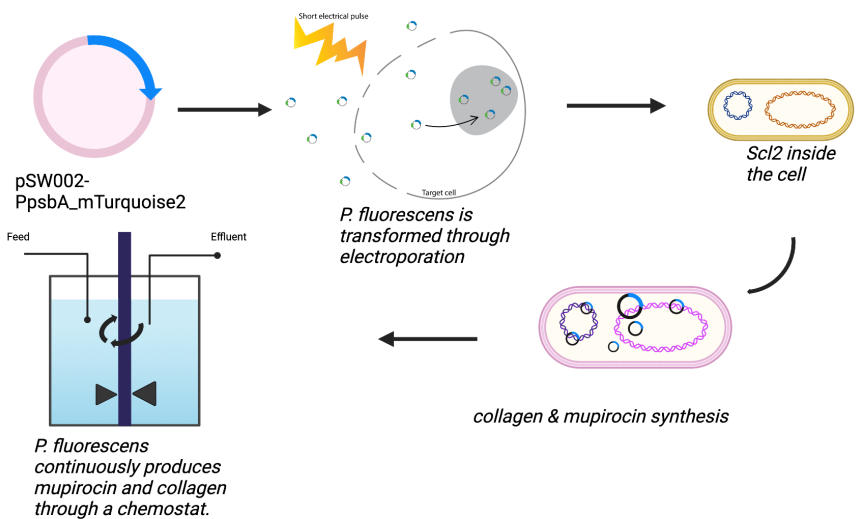
| Figure 4. The process of mass-producing collagen. |
In the plasmid, we will be using the lac1 promoter because of its medium copy ability and the T4 transcription terminator (Figure 5), which regulates the gene expression of recombinant proteins (Wilton et al., 2018).
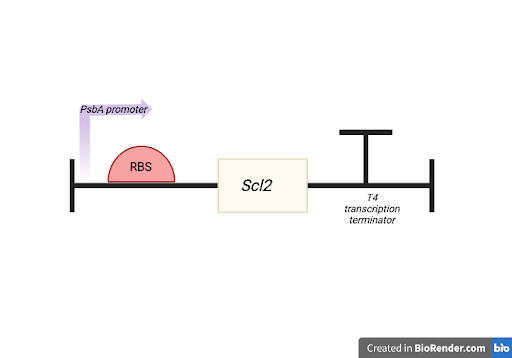
| Figure 5. The collagen binding site. |
The excretion and purification process comprises two major components. First, we will insert the culture of transformed P. fluorescens into a chemostat, a bioprocess that places a bacterial culture in a nutrient chamber that supplies the bacteria with nutrients while harvesting its contents (Abdali et al., 2022). The chemostat automatically extracts all secreted products (e.g. Mupirocin and collagen) from the chamber (Abdali et al., 2022). Second, these byproducts will go through a cross-flow filtration system (Figure 6), which filters out collagen and mupirocin based on their molecular size (Abdali et al., 2022). To quantify the collagen and mupirocin produced by the transformed cultures within the chemostat chamber, we will use the Bradford assay (Figure 7). This laboratory technique measures protein concentration in a given solution based on the light absorbance levels of a dye that binds to the proteins (He, 2011). The dye, Coomassie Blue, is pink in the absence of proteins. After binding to proteins, the dye turns into different shades of blue, which depends on the protein’s light absorbance–therefore concentration– within the solution. In order to determine the concentration of protein in each tube, we will need to make standard concentration curves, which will be used to quantify our results.
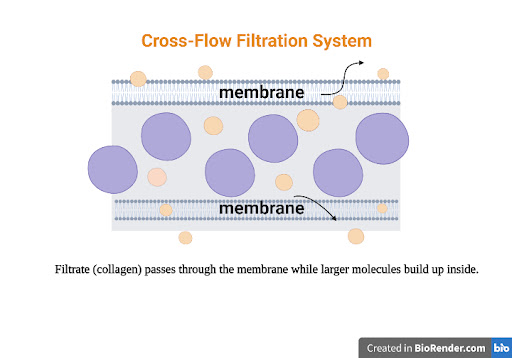
| Figure 6. The Cross Flow Filtration System for Collagen purification. |
The isolated bacterial collagen and mupirocin antibiotic will be the key products in a medicated bandage for patients to treat their burn wounds without the risk of infection. Furthermore, our project ensures that burn patients are not exposed to pathogens, which provides a more viable healing process. This innovative treatment will pave the way to more promising, advanced, and effective care for rehabilitating burn wounds.
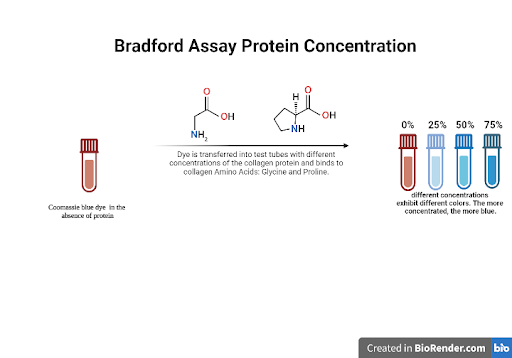
| Figure 7. The Bradford Assay Method; a process used to determine the concentration of collagen and mupirocin. |
Systems level
The pSW002-PpsbA_mTurquoise2 plasmid is electroporated into P. fluorescens, our bacterial vector. Growing the transformed colony in a chemostat allows us to harvest collagen and mupirocin (Figure 4). A chemostat is a bio-processor that harvests a bacterial culture while also supplying it with nutrients. The chemostat is anaerobic and automatically extracts all secreted products from the chamber, including mupirocin and collagen. Next, this solution passes through a crossflow filtration system to filter out collagen and mupirocin based on its molecular size. The his-tag on the plasmid will allow us to identify the collagen protein, giving us a secondary purification method if the crossflow filtration technique is not successful. To quantify the collagen and mupirocin, we then apply the Bradford Assay, a procedure that measures the concentration of protein in a solution. This process helps to determine the total amount of mupirocin and collagen produced.
Device level
To insert Scl2 into the pSW002-PpsbA_mTurquoise2 plasmid and measure mupirocin and collagen, we will use a technique called DNA cloning, which will take place at the ribosome binding site (Figure 5). We will insert the gene in the cloning site between the Ribosome binding site and 6xHistag.
This ligates the Scl2 gene with the plasmid using the EcoR1 restriction enzyme, resulting in a recombinant DNA molecule. After obtaining the transformed plasmid, the next step is to introduce it into P. fluorescens through electroporation. This involves subjecting the bacterial cells to high-voltage electric shocks, which will create temporary pores in the cell membrane and allow the plasmid DNA to enter the cells.
Parts level
We aim to produce the mupirocin antibiotic and exploit the natural production of P. fluorescens combined with the recombinant collagen protein through bacterial transformation. We will utilize the plasmid, which has already been utilized for codon optimization in P. fluorescens. This plasmid contains a PsbA promoter, and a his-tag (Figure 4). Additionally, the plasmid contains a T4 transcription terminator, which will end the transcription of the Scl2 gene. S. pyogenes naturally use this gene to produce a collagen-like protein with a triple-helical structure similar to human-type 1 collagen. The plasmid pSW002-PpsbA_mTurquoise2 also contains the tetracycline resistance gene, which will act as a selectable marker. Since P. fluorescens naturally produces mupirocin, no further steps will be required for its production.
Safety
P. fluorescens is an integral part of our project, as it is our bacterial vector for producing collagen and mupirocin. However, there are risks with using P. fluorescens. It is reported that P. fluorescens can lead to a compromised immunity (Government of Canada, 2021). Mupirocin is the antibiotic we will be using to fight against S. aureus; however, the bacteria can become resistant if applied in large concentrations (Mupirocin, 2021). This is a concern because a burn patient that uses this treatment could become infected because the bacteria would become resistant to the mupirocin. In order to transform the pSW002-PpsbA_mTurquoise2 plasmid into P. fluorescens, electroporation is needed. Electroporation comes with electrical and mechanical hazards. Any electroporation machine produces strong voltage charges that are risky because of electrical shock. The electroporation machine contains safety programming to prevent access to input jacks or other parts that may become charged during the process (MicroPulser Electroporation, n.d.). We are utilizing the Bradford assay technique to measure the collagen concentration in our solution. The Bradford assay uses many different acids and other components that are harmful to the skin, eyes, and organs when made contact with, inhaled or ingested. However, we will follow adequate safety and protection guidelines to prevent injury (Safety Data Sheet, 2017).
Discussion
As we create a final consumer product, we need to consider the risks of testing the medicated bandages on humans. Similarly, to previous studies that tested the efficacy of collagen in tilapia fish skin, our study would require clinical trials to confirm the strength of recombinant collagen that will be produced by P. fluorescens. After this extensive testing and FDA approval, our product would be available for medical use. We also need to consider the risk of bacteria being resistant to our antibiotic, mupirocin. The frequency of mupirocin resistance in Staphylococcus varies depending on the amount of the antibiotic used. To account for this issue, it is critical to ensure optimal levels of the antibiotic are present to treat the infections caused by Staphylococcus. While doing this, we cannot over-use the amounts of mupirocin as it can lead to the development of antibiotic resistance in bacteria. If successful, our collagen production method could be used to generate collagen for treatment of various bone illnesses, including bone malformation diseases, thanks to the benefits collagen has on bone formation and mineralization (Liu, 2014).
The collagen produced could also be used in different industries, such as the beauty industry. Effective anti-aging creams could be produced with bacterial collagen since it has a positive effect on the elasticity of the skin (Bolke et al., 2019). Accessing these benefits with bacterial collagen, instead of animal collagen, will be a huge advancement in cruelty-free medicine and dermatology.
Next steps
Considering that our project proposes a novel and theoretical process for medicated bandages, we will need to test and quantify the produced mupirocin and collagen products. Firstly, we will apply a standard transformation protocol to insert the pSW002-PsbA_mTurquoise2 plasmid, which contains the scl2 gene, into P. fluorescens. After successful transformation, we will move into the production phase. During this crucial step, we will inoculate the chemostat chamber, which will contain the ideal growth medium, with the transformed P. fluorescens.
To properly assess the mupirocin and collagen levels of the chemostat, we will conduct a Bradford assay. Once all of these steps are completed, we will extract collagen and mupirocin using a cross flow filtration system. At this stage of our research process, we are considering basing our medicated bandage on a sheet of cellulose fibers. We have chosen this material for our base, as it has high absorbance, causes little to no skin abrasion, and is widely used in the skincare industry. Our final medicated bandage will also contain adequate amounts of collagen and mupirocin.
Author contributions
A.C., A.L., S.M., O.O., and A.R. conducted the initial research on collagen skin treatments. A.C., A.L., S.M., and A.R. created the project design and completed the paper components. A.C. and S.M. completed the images. A.C., A.L., S.M., O.O., and A.R. edited and produced the video.
Acknowledgments
Our team is grateful for Western Reserve Academy’s continuous support of us through its resources. We would like to acknowledge the work of our peer, Yuejiao (Vivian) Zhou, in the early research process. We extend a special appreciation to our mentor, Dr. Beth Pethel, for introducing us to our love of synthetic biology and expressing continued encouragement in this project.
References
Abdali, Z., Renner-Rao, M., Chow, A., Cai, A., Harrington, M. J., & Dorval Courchesne, N. M. (2022). Extracellular secretion and simple purification of bacterial collagen from Escherichia coli. Biomacromolecules, 23(4), 1557-1568. https://pubs.acs.org/doi/10.1021/acs.biomac.1c01191
Aremu, F. (2021, August 23). Mupirocin, topical treatment. Healthline. https://www.healthline.com/health/mupirocin-topical-ointment
Attinger, C. (2013, July 2). MIST therapy’s effectiveness in wound bed preparation and role of bacterial biofilm in chronic, non-healing wounds (Celleration). ClinicalTrials. https://clinicaltrials.gov/ct2/show/NCT01125735
Florida Springs Institute . (n.d.). Blue tilapia. https://floridaspringsinstitute.org/fish/blue-tilapia/
Florida Fish and Wildlife Conservation Commission. (n.d.). Spotted tilapia. https://myfwc.com/wildlifehabitats/profiles/freshwater/spotted-tilapia
Bolke, L., Schlippe, G., Gerß, J., & Voss, W. (2019). A collagen supplement improves skin hydration, elasticity, roughness, and density: Results of a randomized, placebo-controlled, blind study. Nutrients, 11(10), 2494. http://dx.doi.org/10.3390/nu11102494
Cleveland Clinic. (2022, May 23). Collagen. https://my.clevelandclinic.org/health/articles/23089-collagen
Conde, E. (2019, January 17). Types of skin grafting to cover chronic wounds: Which one should you choose? https://www.elenaconde.com/en/types-of-skin-grafts-to-cover-chronic-wounds-which-one-should-you-choose/
Deane, C. S., Bass, J. J., Crossland, H., Phillips, B. E., & Atherton, P. J. (2020). Animal, plant, collagen, and blended dietary proteins: Effects on musculoskeletal outcomes. MDPI, 12(9). https://doi.org/10.3390/nu12092670
Fischetti, V. A. (2019). Surface proteins on gram-positive bacteria. Microbiology Spectrum, 7(4). https://doi.org/10.1128/microbiolspec.gpp3-0012-2018
Fleck, C. A., & Simman, R. (2010). Modern collagen wound dressings: function and purpose. The Journal of the American College of Certified Wound Specialists, 2(3), 50-54. https://doi.org/10.1016%2Fj.jcws.2010.12.003
Gauglitz, G. G., & Williams, F. N. (2022, April 6). Overview of the management of the severely burned patient. UpToDate. Retrieved January 22, 2023, from https://www.uptodate.com/contents/overview-of-the-management-of-the-severely-burned-patient
Government of Canada. (2021, June 18). Pseudomonas fluorescens – Information sheet. https://www.canada.ca/en/health-canada/services/chemical-substances/fact-sheets/chemicals-glance/pseudomonas-fluorescens.html
He, F. (2011). Bradford protein assay. Bio-Protocol, e45. https://doi.org/10.21769/BioProtoc.45
Henriksen, K., & Karsdal, M.A. (2016). Type I Collagen. In M. A. Karsdal (Ed.), Biochemistry of collagens, laminins and elastin (pp. 1-11). Academic Press. https://doi.org/10.1016/B978-0-12-809847-9.00001-5
Kubala, J. (2022, February). Collagen: Benefits, side effects, and more. Healthline. Retrieved January 22, 2023, from https://www.healthline.com/nutrition/collagen
Lima-Junior, E. M., de Moraes Filho, M. O., Costa, B. A., Fechine, F. V., de Moraes, M. E. A., Silva-Junior, F. R., Soares, M. F. A. D. N., Rocha, M. B. S, & Leontsinis, C. M. P. (2019). Innovative treatment using tilapia skin as a xenograft for partial thickness burns after a gunpowder explosion. Journal of Surgical Case Reports, 2019(6), rjz181. https://doi.org/10.1093/jscr/rjz181
Lima-Júnior, E. M.., de Moraes Filho, M. O., Costa, B. A., Fechine, F. V., Vale, M. L., de Loyola Diógenes, A. K., Neves, K. R. T., Uchôa, A. M. D. N., Soares, M. F. A. D. N., & de Moraes, M. E. A. (2021). Nile tilapia fish skin–Based wound dressing improves pain and treatment-related costs of superficial partial-thickness burns: A phase III randomized controlled trial. Plastic and Reconstructive Surgery, 147(5), 1189-1198. https://doi.org/10.1097/PRS.0000000000007895
Mayo Clinic. (2022, August 13). Burns. https://www.mayoclinic.org/diseases-conditions/burns/diagnosis-treatment/drc-20370545
Mazzei, S. (n.d.). An overview and significance of collagen dressing in
burn. Al Das Medical Clinic. https://www.aldasclinic.com/health-advice/an-overview-and-significance-of-collagen-dressing-in-burn
McIntosh, J. (2023, January 5). Collagen: What is collagen, and why do people use it?. Medical News Today. Retrieved January 22, 2023, from https://www.medicalnewstoday.com/articles/262881
National Cancer Institute (n.d). Extracellular matrix. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/extracellular-matrix
Phelan, H. A., & Bernal, E. (2022, May 18). Treatment of deep burns. UpToDate. https://www.uptodate.com/contents/treatment-of-deep-burns#H2289922971
Seafish. (n.d.). Tilapia. https://www.seafish.org/responsible-sourcing/aquaculture-farming-seafood/species-farmed-in-aquaculture/aquaculture-profiles/tilapia/disease-medicines-and-chemicals/
Sigma-Aldrich. (2017, January 23). Safety data sheet. https://www.geneseo.edu/sites/default/files/users/247/Bradford%20Reagent.pdf
Skin graft information. (n.d.). Mount Sinai. Retrieved January 22, 2023, from https://myfwc.com/wildlifehabitats/profiles/freshwater/spotted-tilapia/#:~:text=Age%20and%20Growth,10%20inches%20typically%20being%20males
Song, W. K., Liu, D., Sun, L. L., Li, B. F., & Hou, H. (2019). Physicochemical and biocompatibility properties of type I collagen from the skin of Nile Tilapia (Oreochromis niloticus) for biomedical applications. Marine Drugs, 17(3), 137. https://doi.org/10.3390/md17030137
Stanford Medicine. (n.d.). Different types of burns. https://stanfordhealthcare.org/medical-conditions/skin-hair-and-nails/burns/types.html
Stewart, B. T. (2022, November 2). Epidemiology, risk factors, and prevention of burn injuries. UpToDate. Retrieved January 22, 2023, from https://www.uptodate.com/contents/epidemiology-risk-factors-and-prevention-of-burn-injuries
Sussman, N. (2017, March 3). Why this Brazilian city uses tilapia fish skin to treat burn victims. PBS NewsHour. https://www.pbs.org/newshour/health/brazilian-city-uses-tilapia-fish-skin-treat-burn-victims
UC San Diego Health. (n.d.). Burn Care. https://health.ucsd.edu/specialties/burn-center/pages/about-burns.aspx
University of Utah Health. (n.d.). Burn surgery. https://healthcare.utah.edu/burncenter/conditions-treatment/surgery.php
Whitaker, P., & Garcia, P. (2017, May 25). Brazilian doctors use fish skin to treat burn victims. Reuters. https://www.reuters.com/article/us-health-brazil-burns/brazilian-doctors-use-fish-skin-to-treat-burn-victims-idUSKBN18L1WH
Wiktor, A., & Richards, D. (2021, July 26). Patient education: Skin burns (Beyond the basics). UpToDate. https://www.uptodate.com/contents/skin-burns-beyond-the-basics
Wilton, R., Ahrendt, A. J., Shinde, S., Sholto-Douglas, D. J., Johnson, J. L., Brennan, M. B., & Kemner, K. M. (2018). A new suite of plasmid vectors for fluorescence-based imaging of root colonizing pseudomonads. Frontiers in Plant Science, 8, 2242. https://doi.org/10.3389/fpls.2017.02242
World Health Organization. (2018, March 6). Burns. https://www.who.int/news-room/fact-sheets/detail/burns Xu, Y., Keene, D. R., Bujnicki, J. M., Höök, M., & Lukomski, S. (2002). Streptococcal Scl1 and Scl2 proteins form collagen-like triple helices. Protein Structure and Folding, 277(30). https://doi.org/10.1074/jbc.M201163200